Charts
Buprenorphine is the most effective office-based treatment available for heroin and prescription opioid addiction
The Problem
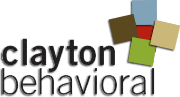
The overdose death rate in Missouri and in the country has been rising for more than 15 years, driven primarily by opioid-related overdoses. Overdose has surpassed car accidents as the leading cause of accidental death in the United States and young adults are especially vulnerable.
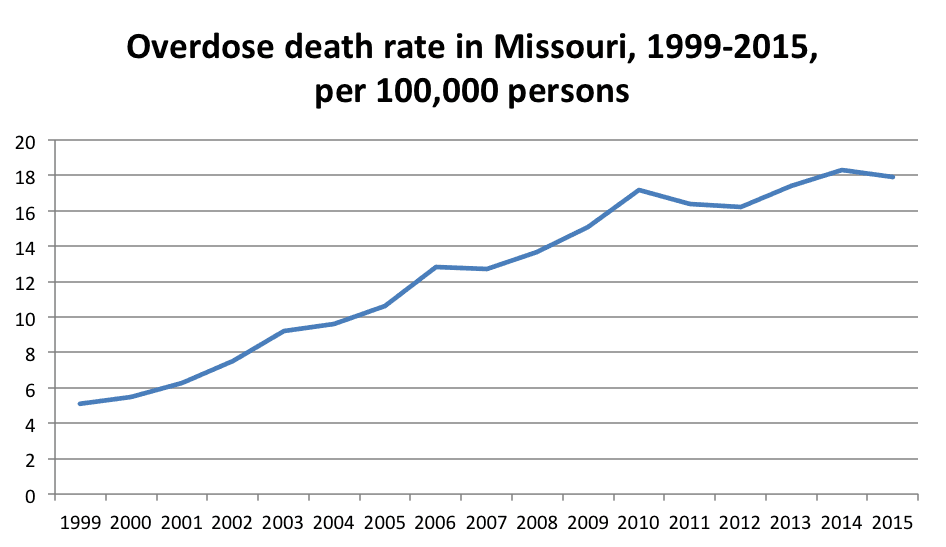
Figure 1. Estimates generated from http://wonder.cdc.gov
Are there solutions?
It is unclear what we will have to do as a state and country to reverse the overdose epidemic. But we can learn from places that have had some success. In 1997, France was concerned about its overdose death rate and began allowing all its physicians to prescribe buprenorphine. About 20% of providers began providing buprenorphine therapy and the overdose death rate decreased 79% over the next few years--in inverse proportion to the number of persons treated with buprenorphine.
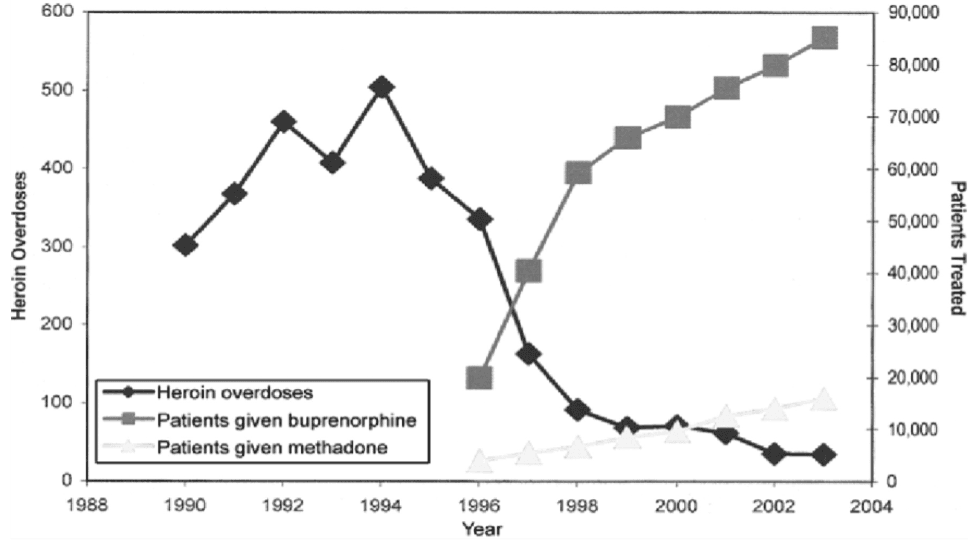
Figure 2. From: Carrieri, Maria Patrizia, et al. "Buprenorphine use: the international experience." Clinical Infectious Diseases 43.Supplement 4 (2006): S197-S215.
The FDA approved buprenorphine in 2003. At that time, Baltimore had the highest overdose death rate in the country. The Baltimore Buprenorphine Initiative was launched to help address the epidemic and in combination with independent buprenorphine providers significantly increased patient access to substitution therapy. As in France, Baltimore observed a drop in its overdose rate inversely proportionate to the increase in buprenorphine patients.
Figure 3. Schwartz, Robert P., et al. "Opioid agonist treatments and heroin overdose deaths in Baltimore, Maryland, 1995–2009." American journal of public health 103.5 (2013): 917-922.
It should be noted that this drop in overdose rate was not sustained, and Baltimore continues to have one of the worst overdose rates in the country. We recently contacted Dr. Schwartz, the lead author on the Baltimore study cited above. When asked why he thought the drop in overdose rate had not been sustained, he said he was unsure. He indicated that the potency of heroin, the widespread presence of fentanyl in heroin samples, and the continued lack of access to substitution therapy could all be factors.
How effective is buprenorphine therapy?
One way to evaluate relative treatment approaches is to consider how successfully the treatment prevents relapse. Researchers examined Medicaid claims from 52,278 beneficiaries in Massachusetts with a diagnosis of Opioid Abuse or Dependence. As a proxy for relapse, they used any insurance claim for detoxification, hospitalization, or Emergency Room visit associated with a Substance Use Disorder (SUD) diagnosis. They compared three types of treatment: methadone, buprenorphine, and non-opioid agonist treatment (non-OAT), i.e. psychosocial only treatment, and tracked relapse events over the course of 36 months.
Methadone and buprenorphine were far more effective in preventing relapse over the course of these three years of treatment. In examining the results, one should keep in mind that each relapse carries with it a significant risk for death.
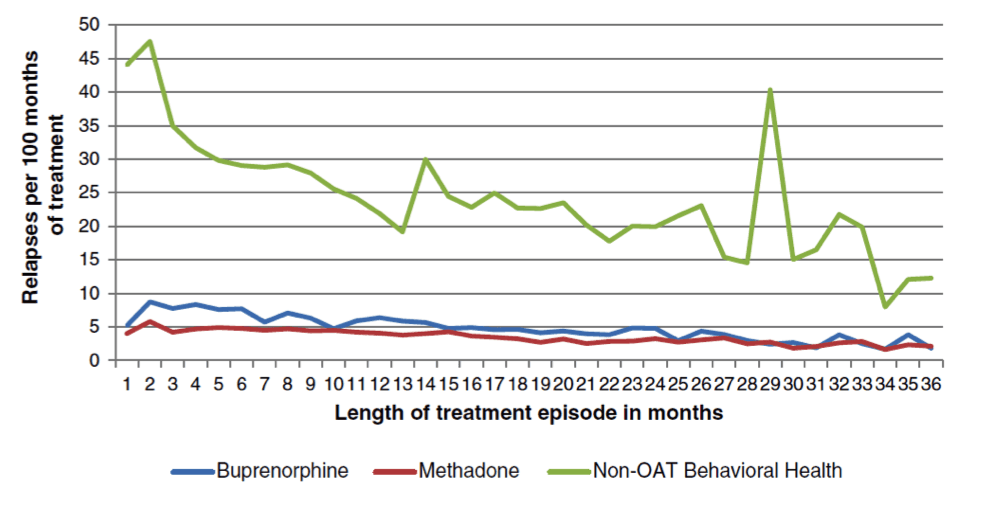
Figure 4. Clark, Robin E., et al. "Risk factors for relapse and higher costs among Medicaid members with opioid dependence or abuse: opioid agonists, comorbidities, and treatment history." Journal of substance abuse treatment 57 (2015): 75-80.
This chart only includes persons who were retained in treatment at each time point. At 12 months, 52% of methadone patients, 33% of buprenorphine patients, and 12% of non-OAT patients had been retained in treatment.
Should we be using buprenorphine for detox rather than maintenance?
Perhaps the most common misconception about buprenorphine is that it is better used for detoxification than maintenance. In one study, 154 youth with opioid dependence were randomized to a 14-day detoxification taper or 9 weeks of maintenance followed by a 21-day taper. All received weekly individual and group counseling at minimum. At Week 4, 84% of patients in the maintenance group had been retained and 74% of those had been opioid abstinent in the past week; in the detox group, 21% had been retained and 37% of those had been opioid abstinent in the past week. Maintenance was much more effective at both retaining patients and helping them eliminate opioid use.
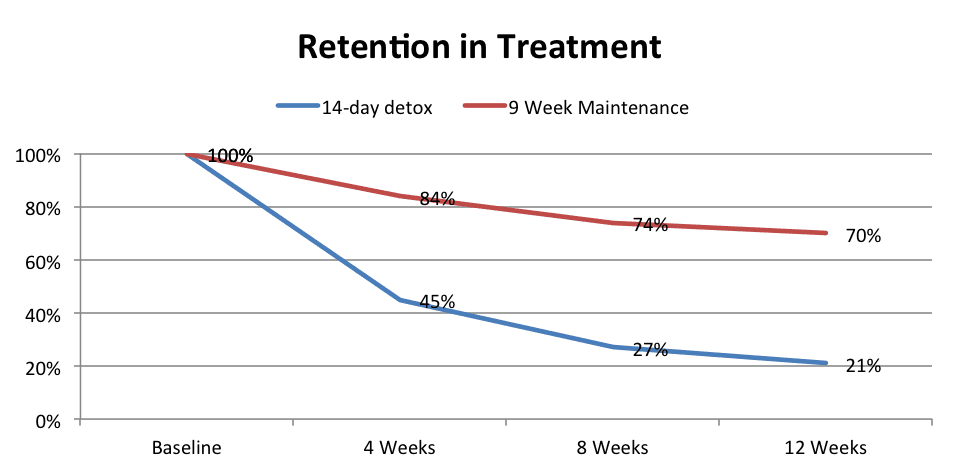
Figure 5. Woody, George E., et al. "Extended vs short-term buprenorphine-naloxone for treatment of opioid-addicted youth: a randomized trial." Jama 300.17 (2008): 2003-2011.
Perhaps even more telling than the superior effectiveness of short-term maintenance is that the moment the maintenance group began to be tapered, they also began relapsing to opioid use, eliminating the positive effects of the brief maintenance therapy.
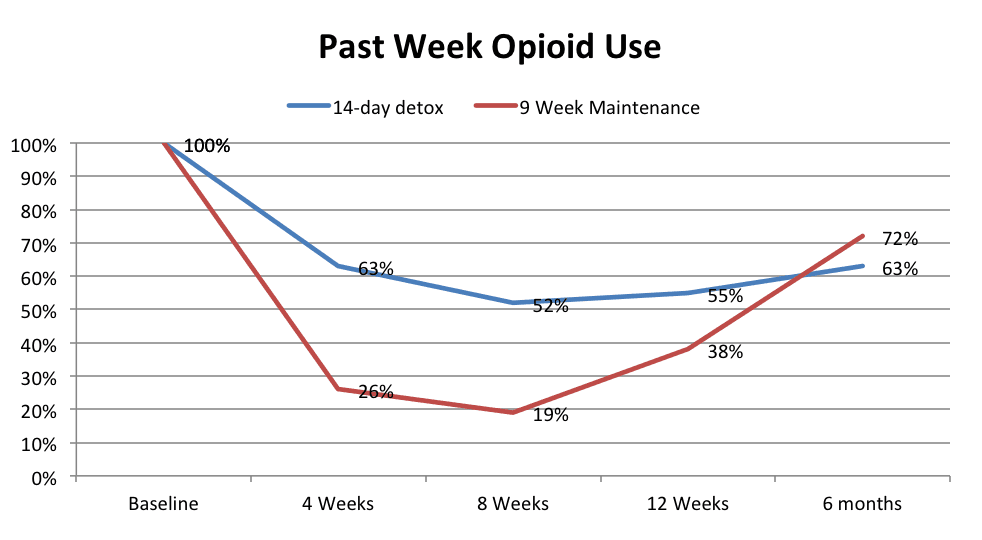
Figure 6. Woody, George E., et al. "Extended vs short-term buprenorphine-naloxone for treatment of opioid-addicted youth: a randomized trial." Jama 300.17 (2008): 2003-2011.
What if detoxification is followed by XRT naltrexone (Vivitrol)?
The first problem with buprenorphine detoxification followed by XRT naltrexone is that many patients drop out during detoxification and never receive an injection of XRT naltrexone. Proponents of XRT naltrexone recently circulated an article comparing detox protocols prior to XRT naltrexone induction. In the following chart, I include retention rates for these protocols along with the retention for a 16mg maintenance dose of buprenorphine. The data on buprenorphine maintenance comes from a multisite randomized controlled trial of buprenorphine dosing.
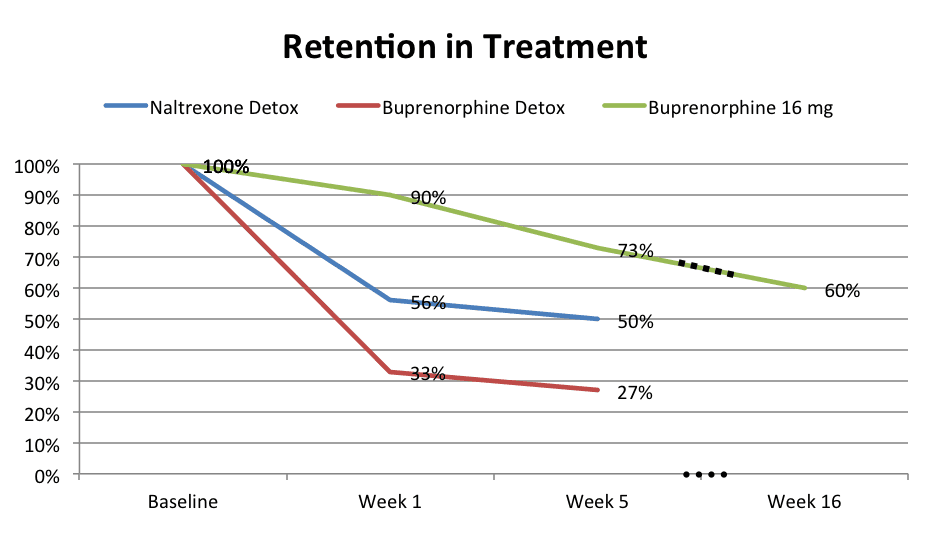
Figure 7. Sullivan, Maria, et al. "Long-Acting Injectable Naltrexone Induction: A Randomized Trial of Outpatient Opioid Detoxification With Naltrexone Versus Buprenorphine." American Journal of Psychiatry (2017): appi-ajp.
Maintenance dosing is much more effective in retaining patients than detox + XRT naltrexone, but the comparison above is actually biased against the maintenance protocol. In the buprenorphine study, patients were addicted to heroin. In the XRT naltrexone study, 37% of the patients were primarily addicted to prescription opioids, and patients addicted to heroin were 2.31 times less likely than those with prescription opioid dependence to receive the Week 5 XRT naltrexone injection. In other words, patients with heroin addiction in the superior detox protocol had a Week 5 retention rate significantly lower than 50%. Compare that with the buprenorphine maintenance protocol which had a Week 16 retention rate of 60% in persons with heroin dependence. Is there something so compelling about antagonist medication that we are willing to lose one third to one half of our patients to attrition in order to prioritize its use?
To date, there is no study showing equal or superior outcomes for XRT naltrexone when compared with buprenorphine maintenance for opioid dependence. A second problem with XRT naltrexone is that persons who are successful in XRT naltrexone treatment lose their tolerance to opioids and become highly vulnerable to overdose death. This increased risk for death has made many clinicians very wary of Vivitrol treatment.
In short, buprenorphine maintenance is the best office-based treatment available to persons with heroin and prescription opioid addiction. It is convenient, effective, and can help support long-term recovery.
i Carrieri, Maria Patrizia, et al. "Buprenorphine use: the international experience." Clinical Infectious Diseases 43.Supplement 4 (2006): S197-S215.
ii Schwartz, Robert P., et al. "Opioid agonist treatments and heroin overdose deaths in Baltimore, Maryland, 1995–2009." American journal of public health 103.5 (2013): 917-922.
iii Clark, Robin E., et al. "Risk factors for relapse and higher costs among Medicaid members with opioid dependence or abuse: opioid agonists, comorbidities, and treatment history." Journal of substance abuse treatment 57 (2015): 75-80.
iv Woody, George E., et al. "Extended vs short-term buprenorphine-naloxone for treatment of opioid-addicted youth: a randomized trial." Jama 300.17 (2008): 2003-2011.
v Sullivan, Maria, et al. "Long-Acting Injectable Naltrexone Induction: A Randomized Trial of Outpatient Opioid Detoxification With Naltrexone Versus Buprenorphine." American Journal of Psychiatry (2017): appi-ajp.
vi Comparsion study: Ling, Walter, et al. "Buprenorphine maintenance treatment of opiate dependence: a multicenter, randomized clinical trial." Addiction 93.4 (1998): 475-486.
Download this page PDF version
Contact Us
9890 Clayton Rd, Suite 100
St. Louis, MO 63124
Annex
9904 Clayton Road, Suite 135
St. Louis, MO 63124